Covid Testing Covered By Insurance Aetna
The Families First Coronavirus Response Act and CARES Act do not require an insurance company to pay for a test unless you have symptoms or a known or recent exposure to COVID-19 and it has been determined to be medically necessary for you by an attending healthcare provider. While the government has made proclamations that COVID testing will be covered the same isnt true for treatment.
Epo Health Insurance Plans From Aetna Exclusive Provider Organization Health Care Coverage
Other insurers have committed to covering testing at no cost to patients as well as treatment from doctor visits.

Covid testing covered by insurance aetna. Thats because federal law requires insurers to waive costs for covid testing and. Visit our COVID-19 FAQ page for answers to the most frequently asked questions regarding the coronavirus and to get the latest information. Carriers in Nebraska regarding the Coronavirus also known as COVID-19.
Repeated Covid-19 testing is going to be a part of public life for the foreseeable future. Aetna providers can deliver and receive reimbursement for telemedicine services provided through video. Utah Insurance Department COVID-19 Coverage Survey March 17 2020 Insurer.
For covid through Aetna. Though many airlines including Air Canada and WestJet and insurance companies like Manulife Allianz and Blue Cross are already offering COVID-19. Insurers like Cigna Aetna Kaiser Permanente UnitedHealth Group and Humana have announced they will waive some out-of-pocket costs for COVID-19 treatment.
No precertification will be needed. Learn more about Aetnas coverage policies and guidelines for COVID-19 testing treatment and pricing for patients and providers. Visit our FAQ page for answers to the most frequently asked general questions and concerns regarding COVID-19 and to get the latest information.
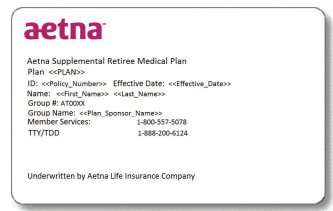
If you have Aetna health insurance you can visit their site here to review Testing Treatment FAQs which include details about coverage and authorizations for COVID-19 expenses. Most health insurance providers have waived costs related to the testing and treatment of COVID-19. Treatment co-pays and co-insurance Dozens.
With over 100 million cases of coronavirus disease recorded in almost every country in the world it is now certain that COVID-19 is and will be present in our lives for quite some time now. Washington Tests to detect antibodies in people who have previously been infected by the coronavirus must be covered free of charge under health insurance plans and Medicaid according to. Subscribe to International Investments free daily newsletter Previous Article.
Learn about extra benefits and well-being resources just for you find testing locations get answers to the most frequently asked questions regarding COVID-19 and tips to stay safe and much more. We suggest you check directly with them to learn more about your coverage. Coronavirus and Global Health Insurance Benefits.
People covered by insurance plans those bought by individuals. This could change if theres more evidence about antibody testing but were currently only covering antibody testing for the uses listed above. Aetna will waive co-pays for all diagnostic testing related to COVID-19 according to CVS Health.
Up to and including 31 March 2021 Aetna International members will be covered for one test per calendar month if they are asymptomatic and classified as high-risk - as referred by a medical practitioner and when testing takes place in an appropriate medical facility. Aetna will cover CDC recommended physician-ordered testing for COVID-19. Visits are cash-only and not covered by insurance.
Aetna will waive co-pays for all SARS-CoV-2 testing for all insured enrollees whether the. Under the terms of the families first coronavirus response act hr6201 medicare medicaid and private health insurance plans including grandfathered plans are required to fully cover the cost of covid-19 testing without any cost-sharing or prior-authorization requirements for the duration of the emergency period which has most. Insurance Non-Covered for Rapid COVID Test Medicaid Keystone First Health Partners Aetna Better Health UHC Community Plan Generally Rapid COVID-19 testing is not covered but standard NAA testing is usually covered.
Members Aetna is here to keep you informed during the coronavirus COVID-19 pandemic. Medicaid Keystone First Health Partners Aetna Better Health UHC Community Plan Generally Rapid COVID-19 testing is not covered but standard PCR testing is usually covered. Members Aetna is here to keep you informed during the coronavirus COVID-19 pandemic.
Max Sullivan Aetna is among the first national insurance companies to waive cost-sharing and co-pays for inpatient hospital admissions related to COVID-19. Members Aetna is here to keep you informed during the coronavirus COVID-19 pandemic. Aetna is here for you during the coronavirus COVID-19 pandemic no matter what.
Medicaid patients may not pay out of pocket for Rapid COVID Testing. Visit our FAQ page for answers to the most frequently asked questions regarding COVID-19 testing and treatment and to get the latest information. The following insurers and their responses to COVID-19 can be found below and will be updated when new information is provided by insurers.
Medicaid patients may not pay out of pocket for Rapid COVID Testing Generally only. That includes all member costs associated with diagnostic testing for Commercial Medicare and Medicaid lines of business. Tests are only covered for members experiencing late complications of COVID-19 illness when administered in an emergency room observation setting or inpatient setting.
Self-insured plan sponsors will be. Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. The current regulatory arrangement creates the opportunity for industrial-grade fraud.
Medicaid will cover the full cost of COVID-19 testing for the uninsured as directed by the CARES Act. Aetna providers we are here to support you during the coronavirus pandemic with timely answers to the most frequently asked questions about state testing information and other patient care needs.
Coronavirus Covid 19 Taking Action Aetna

Cvs Health Announces Availability Of Covid 19 Antibody Testing At Minuteclinic Locations Across The Country Cvs Health
Coronavirus Covid 19 Allina Health Aetna
Extra Member Benefits During The Coronavirus Outbreak Aetna
Health Care Plan Benefits Human Resources Vanderbilt University

Aetna Cigna And Humana Waive Most Costs To Patients For Covid 19 Treatment Shots Health News Npr

Covid Testing Care Station Medical Group

Covid 19 Testing Bills Surprise New Yorkers Crain S New York Business

Coronavirus Covid 19 Allina Health Aetna

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

What To Know About Coronavirus Your Insurance Utah Insurance Department

Coronavirus Covid 19 Resources Aetna Medicaid Illinois

Covid 19 Resources Support For Aetna Providers
Covid 19 Services Promptmd Hoboken Edgewater Jersey City Nj

Coronavirus Covid 19 Resources Aetna Medicaid Illinois

Coronavirus Covid 19 Allina Health Aetna
Posting Komentar untuk "Covid Testing Covered By Insurance Aetna"