Does Insurance Cover Rapid Covid Tests
We cover without member cost sharing a same day office emergency room or other provider visit at which a COVID-19 test is ordered or administered. Americas Health Insurance Plans is calling on more government support to cover the cost of COVID-19 tests which it says could be between 6 billion and 25 billion annually.

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
Tests must be provided or ordered by a healthcare provider licensed or authorized to provide or order COVID-19 tests.

Does insurance cover rapid covid tests. This requirement not only includes the cost of the test itself but also the cost of any related office urgent care emergency room or telehealth visits. Yes Medicare Part B medical insurance covers all costs for tests to see whether you have COVID-19. Routine testing for influenza strep and other respiratory infections without a COVID-19 test will be covered subject to applicable cost sharing under the members plan.
When tests are available for you in your state Medicare covers and you pay nothing for. Rapid Point of Care Testing. The rapid test at Walgreens is listed at 49 total.
As of Wednesday Dec. 2 Walgreens website listed its additional charge as 29 and CVS listed a 39 extra charge for the PCR test. Blue Shield and Blue Shield Promise cover these diagnostic tests.
You dont need an order from a doctor and youre covered for tests you get from a. Insurers are legally required to pay for in-network testing so try to find a medical facility where you know youll be covered. You do not need to obtain a referral from a physician in order to get a COVID-19 test and have it covered by Medicare.
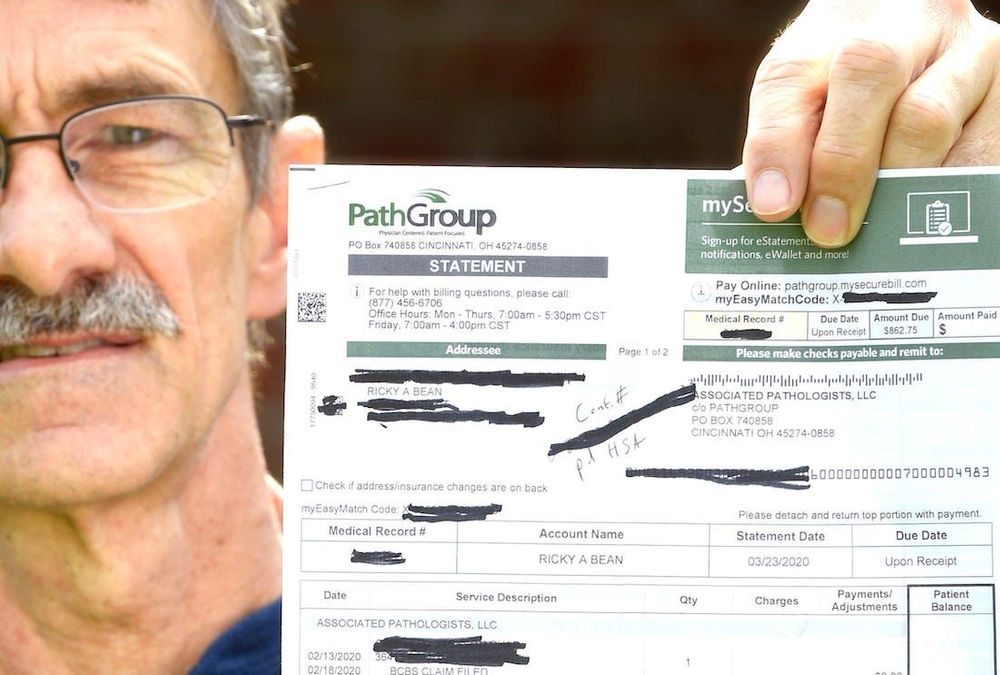
At the day of your rapid test please make sure you have insurance and ID ready and register at the front desk. On top of that there may also be costs associated with the office or clinic visit. 2 Rapid-result tests can be pricey costing up to 250 and often arent covered by health insurance.
Medicare covers these tests at different locations including some parking lot test sites. Based on information gathered from the five largest health insurance companies in the United States there is no limit on how many free COVID-19 tests an insured member can receive. Under the Act public and private insurance including self-funded plans have to cover FDA-approved coronavirus tests.
For example tests conducted for return to work purposes or travel are generally not covered. Youll need a negative COVID-19 viral test to re-enter the United States as well. Medicare reimburses up to 100 for the COVID test.
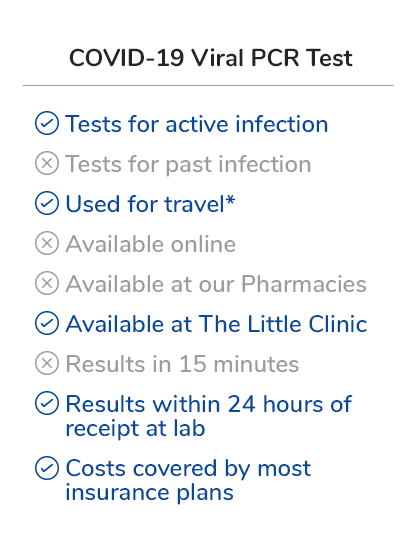
How does the COVID-19 rapid test process work at AFC. Many airports are now offering test sites. Standard PCR tests sent to a lab.
When are COVID-19 tests. Tests to diagnose or aid the diagnosis of COVID-19. UnitedHealthcare will cover FDA-authorized rapid point of care virusantigen detection and antibody testing.
Both the FFCRA and the CARES Act contain requirements that group and individual health insurance plans cover COVID-19 diagnostic testing without cost-sharing co-pays or deductibles. Most health insurance plans do not cover COVID-19 tests for reasons other than diagnosis or treatment by a health care professional. There is no appointment needed.
Since the legislation was passed on March 18 2020 all forms of public and private insurance are required to cover the costs of COVID-19 testing using tests approved by the FDA so long as the. Many insurers have also agreed to cover the cost of a COVID test if its done at an out-of-network facility but youll want to reach out to your insurance company or MedicareMedicaid provider before your visit. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test.
Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings. UnitedHealthcare is also waiving cost sharing for COVID-19 testing-related services received in-person or via telehealth for the following health plans. Some that charge travelers for rapid and PCR tests and some that offer complimentary screenings for travelers.
Getting your rapid test is a quick and easy process. The Families First Coronavirus Response Act and CARES Act do not require an insurance company to pay for a test unless you have symptoms or a known or recent exposure to COVID-19 and it has been determined to be medically necessary for you by an attending healthcare provider. Rapid point of care antigen tests where results are available within a few minutes Home test kits when ordered by a licensed healthcare provider.
Rapid Covid 19 Test Available All Locations Mydoc Urgent Care

How Americans Can Get A Covid Test In Mexico The Washington Post
.png)
News Covid 19 Testing Sites For Newark Residents

If You Get A Coronavirus Test Will Insurance Pay It Depends Shots Health News Npr
Texas Medclinic Offers Rapid Covid Testing Near Me Walk In Clinic

Covid 19 Testing And Covid Antibody Testing Stat Med Urgent Care
Launching Rapid Covid 19 Tests Mydoc Urgent Care

Differences Between Rapid Pcr Tests Physicianone Urgent Care
What Is A Rapid Antigen Test How Is It Different From Other Covid 19 Tests Abc News

Binaxnow Covid 19 Antigen Self Test At Home Kit Walgreens
How Much Does A Rapid Covid 19 Test Cost Without Insurance Mira
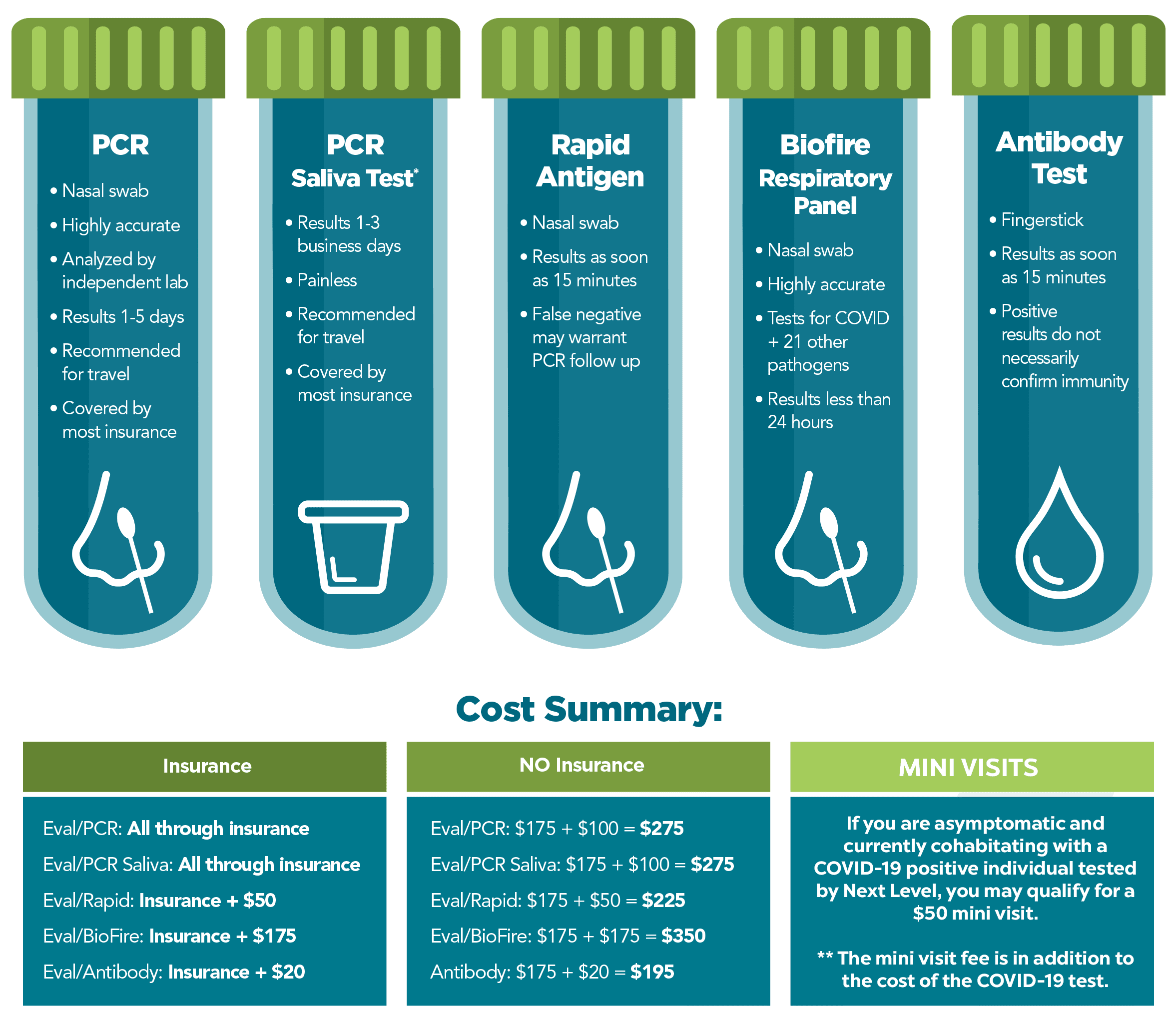
Covid 19 Testing Next Level Urgent Care
Pharmacy Hours Online Services Coronavirus Updates City Market
Rapid Covid 19 Tests Mydoc Urgent Care

Covid 19 Testing Healthcare Services In New York Multi Specialty Practices
Private Health Coverage Of Covid 19 Key Facts And Issues Kff

How Home Coronavirus Testing Could Slow Disease Spread

Rapid Covid Tests What You Should Know About Accuracy

Chicago Covid Testing Rapid Covid 19 Tests Drive Up Screening Clinic
Posting Komentar untuk "Does Insurance Cover Rapid Covid Tests"