How Often Does Insurance Cover Covid Testing
You do not need to obtain a referral from a physician in order to get a COVID-19 test and have it covered by Medicare. Additional member guidance on testing can be found here.
.png)
News Covid 19 Testing Sites For Newark Residents
Or if a factory tests workers every two weeks.
/cloudfront-us-east-1.images.arcpublishing.com/gray/GZYXYQYUUZDIJBOHB7O2GFD6HE.png)
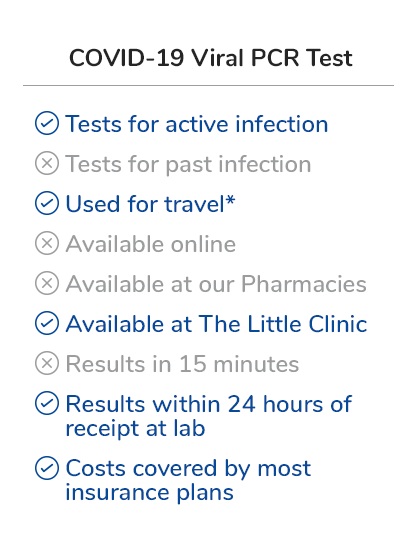
How often does insurance cover covid testing. Youd also owe 20 percent of the Medicare-approved cost for physicians services while youre an inpatient after the 198 Part B deductible. Covers a COVID-19 antibody or serology test. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test.
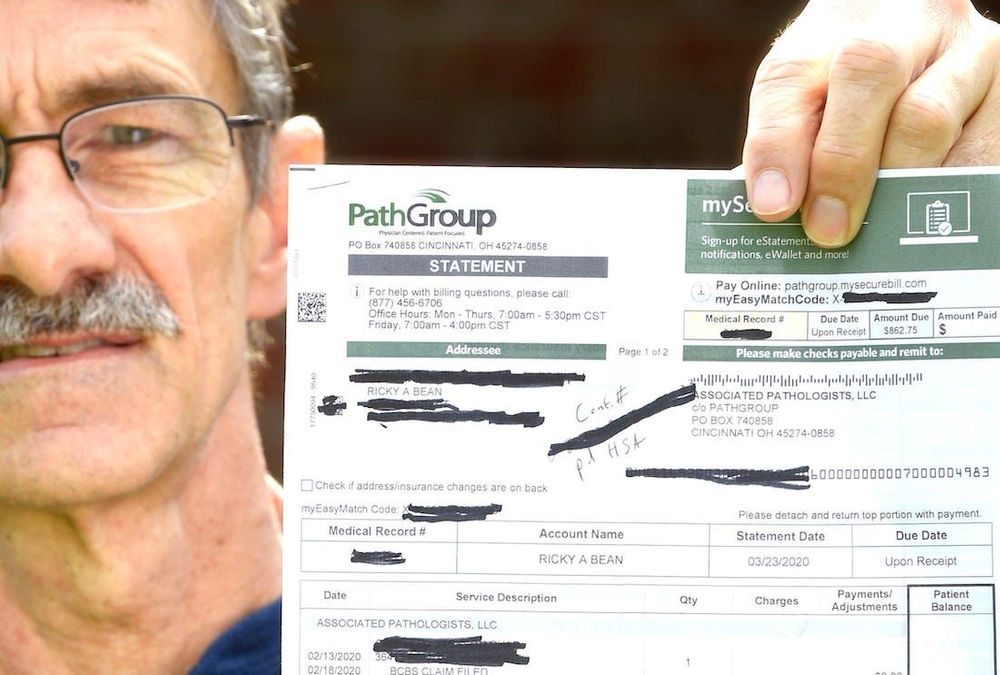
Stays ranged from seven to 14 days. Tests to diagnose or aid the diagnosis of COVID-19. Effective March 20 2020 the Ohio Department of Insurance issued a bulletin defining.
Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a. Who pays when all employees are required to have a negative COVID test in order to return to work. All airline passengers to the United States ages two years and older must provide a negative test taken within three calendar days of travel or documentation from a licensed health care provider showing youve recovered from COVID-19 in the 90 days preceding travel.
Several health insurance companies reached an agreement with the state to waive co-payments co-insurance and deductibles for COVID-19 testing. What Travel Insurance Does Not Cover Related to COVID-19. If you have health care coverage directly from an insurance company the health insurance marketplace or through your employer including through COBRA.
When tests are available for you in your state Medicare covers and you pay nothing for. Tests for the coronavirus are covered by Medicare Part B much like many other tests and screenings. Medicare covers these tests at different locations including some parking lot test sites.
The out-of-pocket cost for a travel test is. Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles. COVID testing for travel gets complicated doesnt it.
If you have a short-term medical plan do the research. A study from Wuhan China found people hospitalized for COVID-19 have an average stay of 11 days. The Departments of Health and Human Services Labor and the Treasury originally interpreted testing coverage requirements laid out by the Families First Coronavirus Response Act FFCRA.
Ohio Department of Health Director Amy Acton MD MPH strongly recommends that Ohioans are aware of the following information provided by the Ohio Department of Insurance regarding out-of-network insurance coverage specific to COVID-19 testing and treatment. Standard travel insurance does not cover trip cancellation due to fears or concerns about traveling during the coronavirus pandemic or any other epidemic. UnitedHealthcare will cover COVID-19 testing for all lines of business in accordance with the members benefit plan.
And second youre in luck. Review the frequently asked questions below about the health insurance order for more information. Standard travel insurance will not offer trip cancellation for government mandated travel restrictions either.
C ontact your insurance company. Youll need a negative COVID-19 viral test to re-enter the United States as well. Members should work with their provider to order a test.
Based on information gathered from the five largest health insurance companies in the United States there is no limit on how many free COVID-19 tests an insured member can receive. The other type of insurance that may not cover testing is short-term medical. Out-of-pocket testing costs for COVID-19 individual diagnostic tests will be waived during the federal public health emergency.
For Medi-Cal members all tests are fully covered at no cost to members. Many times testing will be covered but dont assume it is. If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare.
Health insurers are not required to cover COVID-19 testing for employer or surveillance-related purposes alone three agencies clarified in new guidance this week. Original Medicare covers COVID-19 testing with no out-of-pocket Medicare costs to you. The travel test is self-pay as such tests are often not considered to be medically necessary and therefore typically not covered by health insurance.
This will continue as long as state and federal mandates for the coverage of testing without out-of-pocket costs apply. COVID-19 testing would continue to be covered with no cost-sharing by private and public insurers for all tests consumers independently seek but the federal government would pay directly for. All private insurance has to cover 100 of the cost of COVID-19 testing Pollitz said she is miffed that employers are trying to argue otherwise.
Still its happening and not only in. Medicare Part B Medical Insurance Part B covers certain doctors services outpatient care medical supplies and preventive services. State variations and regulations may apply.
Information on the COVID-19 webpages changes frequently and is updated regularly. Coronavirus disease 2019 COVID-19 antibody test. Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021.
Waiving cost-sharing for COVID-19 testing and treatment. That means members will pay nothing out-of-pocket to take care of their COVID-19-related health needs. Through May 31 all BCBS companies including the BCBS Federal Employee Program FEPare.
A test must be covered if your attending health care provider has assessed your individual situation and determined that it is medically appropriate you have symptoms or have a known or likely recent exposure to COVID-19.
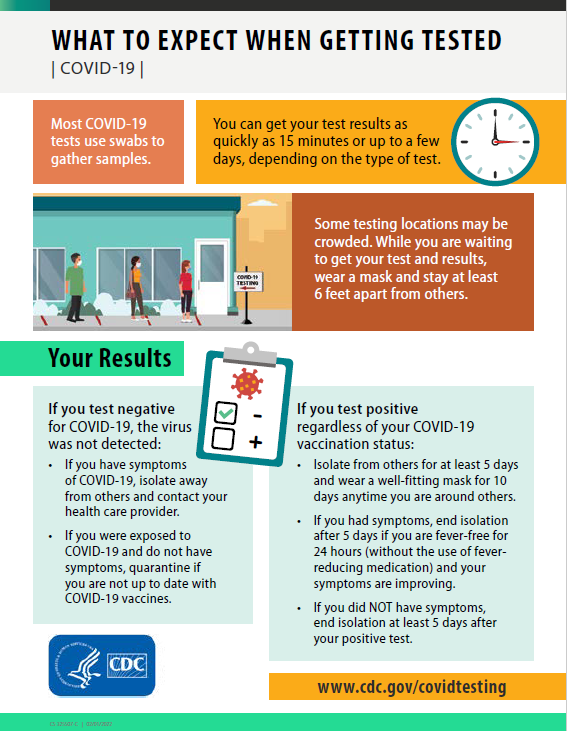
Testing Communication Toolkit Cdc

Rapid Covid Tests What You Should Know About Accuracy
/cloudfront-us-east-1.images.arcpublishing.com/gray/GZYXYQYUUZDIJBOHB7O2GFD6HE.png)
Free Walgreens Drive Thru Testing Site To Open Aug 7

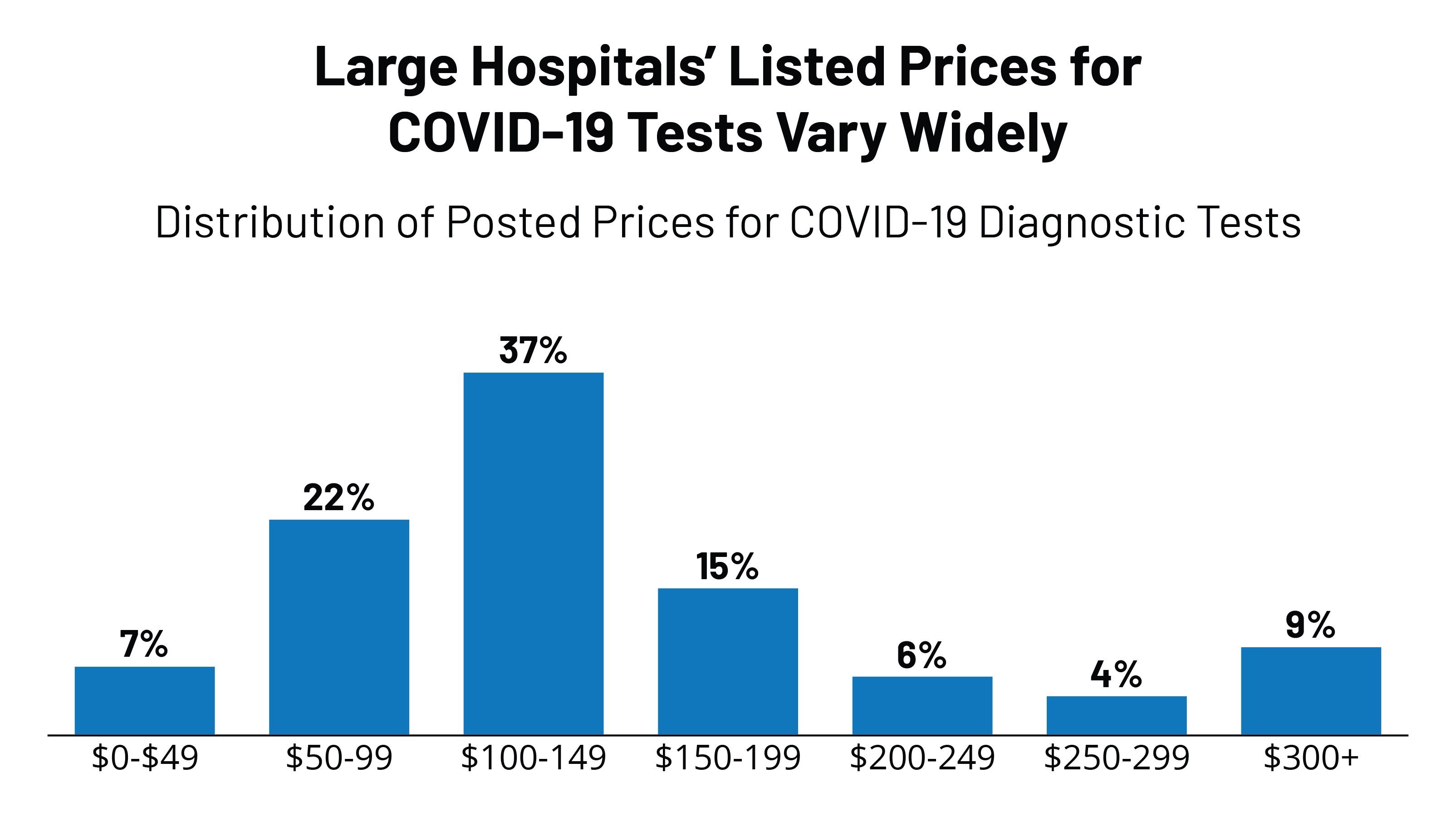
Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff
Test Trace Corps Testing Nyc Health Hospitals
Pharmacy Hours Online Services Coronavirus Updates Kroger

Nuevas Pruebas De Covid 19 Sin Ir A Un Laboratorio
State Covid 19 Data And Policy Actions Kff
Covid 19 Testing Results Albany County Ny

Covid 19 Testing Anne Arundel County Department Of Health

Covid Insurance For Foreigners In Thailand

Testing Communication Toolkit Cdc

Covid 19 Information Medstar Health System

How Americans Can Get A Covid Test In Mexico The Washington Post
How Much Does A Rapid Covid 19 Test Cost Without Insurance Mira
![]()
Covid 19 Test Prices And Payment Policy Peterson Kff Health System Tracker
Covid 19 Testing Tufts Medical Center

Posting Komentar untuk "How Often Does Insurance Cover Covid Testing"