Does Health Insurance Cover The Rapid Covid Test
At-home tests obtained without a doctor or providers order are not covered. During the public health emergency there will be no out-of-pocket costs for Humana Medicare Advantage and Medicaid members who receive a US Food Drug Administration FDA approved or emergency use authorized COVID-19 test opens new window.

Covid 19 Rapid Antigen Test Available Curbside Urgent Care Clinic
Department of the Treasury jointly prepared.
Does health insurance cover the rapid covid test. Medicare covers the necessary testing for the novel coronavirus completely free of charge. Additional testing sites may be available in your area. Some tests for related respiratory conditions to aid diagnosis of COVID-19 done together with the COVID-19 test.
State variations and regulations may apply. COVID-19 tests are available at no cost nationwide at health centers and select pharmacies. Its 219 for same-day results or 299 for results in one hour.
Will Humana cover Covid-19 testing. Federal law requires all private insurance plans to cover the entire cost associated with approved COVID-19 testing so long as the test is deemed medically appropriate. Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show symptoms or tests are ordered by a.
Medicare reimburses up to 100 for the COVID test. Coronavirus COVID-19 Health Insurance FAQs. Humana Commercial Group members.
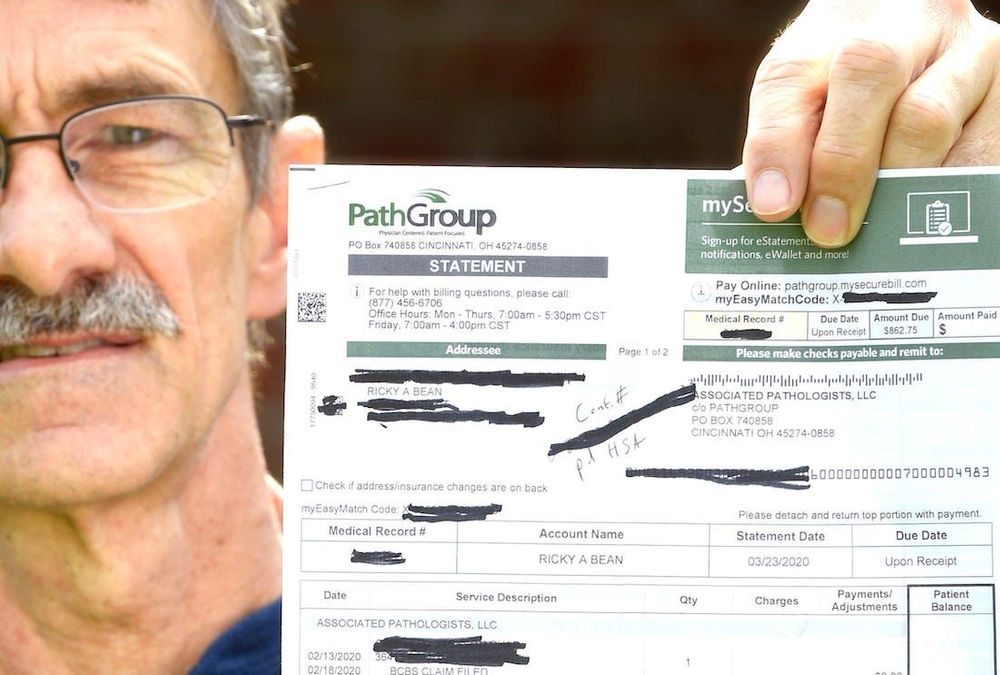
Medicare covers these tests at different locations including some parking lot test sites. Tests to diagnose or aid the diagnosis of COVID-19. 2 Rapid-result tests can be pricey costing up to 250 and often arent covered by health insurance.
Blue Shield and Blue Shield Promise cover these diagnostic tests. Government pre-paid for COVID-19 vaccines and required COVID-19 vaccines be made available at no out-of-pocket costs regardless of whether the vaccine. Standard PCR tests sent to a lab.
The Families First Coronavirus Response Act ensures that COVID-19 testing is free to anyone in the US including the uninsured. Most health insurance plans do not cover COVID-19 tests for reasons other than diagnosis or treatment by a health care professional. Employers have more clarity on COVID-19 testing coverage requirementsincluding new details on at-home tests return-to-work testing and out-of-network pricingunder new guidance that the US.
When are COVID-19 tests not. COVID-19 Testing Guidance. And the price is widely variable in the private market.
UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. Many people who contract the novel coronavirus may. Tests must be provided or ordered by a healthcare provider licensed or authorized to provide or order COVID-19 tests.
Employer sponsored self-funded health plan are regulated by the US Department of Labor under ERISA. Whether you conduct your COVID-19 test at home or at a clinic if its ordered by a licensed health care professional who believes its medically appropriate then federal legislation requires your private health plan to cover the cost said Sabrina Corlette a research professor who studies health insurance policy at the Center on Health Insurance Reforms at Georgetown University. And over at Allianz Global Assistance which offers COVID-19 insurance and assistance for clients who test positive for COVID-19 while travelling a COVID-19 test will only be.
Federal law requires insurers to fully cover the tests when ordered by a. Many airports are now offering test sites. These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan.
UnitedHealthcare will cover medically appropriate COVID-19 testing during the national public health emergency period currently scheduled to end Oct 17 2021 at no cost share when ordered or reviewed by a physician or appropriately licensed health care professional to either. HealthPartners covers COVID-19 diagnostic tests when theyre 1 ordered by a doctor or appropriately licensed provider AND 2 for medically necessary purposes. Department of Labor DOL and the US.
Some that charge travelers for rapid and PCR tests and some that offer complimentary screenings for travelers. Dean Health Plan will cover the test and doctor visit at no cost to members when the basis for the visit is related to testing for COVID-19. On top of that there may also be costs associated with the office or clinic visit.
Doctors typically charge about 50 to 100 for the tests so the costs of weekly testing could add up quickly. If your doctor or other health care professional provides a prescription or order for the over-the-counter COVID-19 test as part of clinical care you may submit a claim for reimbursement with both the prescription and detailed receipt to UnitedHealthcare. Youll need a negative COVID-19 viral test to re-enter the United States as well.
Tufts Medical Center conducts tests in Boston with results in 48-72 hours. If your insurance does not cover the test the cost is 135. When tests are available for you in your state Medicare covers and you pay nothing for.
Department of Health and Human Services HHS US. Delta Dental of Iowa and the Delta Dental of Iowa Foundation have committed 105 million in grants to COVID-19 relief programs to help Iowa dentists and nonprofits. Those self-funded employer plans do not have to conform to any.
Based on information gathered from the five largest health insurance companies in the United States there is no limit on how many free COVID-19 tests an insured member can receive. Humana Medicare Advantage and Medicaid members. Delta Dental of Arizona.
Rapid point of care antigen tests where results are available within a few minutes Home test kits when ordered by a licensed healthcare provider. The Connecticut Department of Insurance regulates fully insured health insurance plans issued in the State of Connecticut only. For example tests conducted for return to work purposes or travel are generally not covered.
Since the legislation was passed on March 18 2020 all forms of public and private insurance are required to cover the costs of COVID-19 testing using tests approved by. DM Covid-19 Test conducts curbside tests at their Columbia office.

Mass Testing For Covid 19 January Update On Lateral Flow Tests Post

Millions Of At Home Covid Rapid Tests Risk Going Uncounted By Us Bloomberg

How Americans Can Get A Covid Test In Mexico The Washington Post

Most Affordable Covid 19 Rapid Diagnostic Test Now Available Unicef Supply Division

Differences Between Rapid Pcr Tests Physicianone Urgent Care

Rapid Covid 19 Testing Vitalcare Primary And Family Care

Sars Cov 2 Covid 19 Diagnosis By Igg Igm Rapid Test Clinisciences

Why At Home Rapid Covid Tests Cost So Much Quartz

How Much Does A Covid 19 Test Cost To Travel To Spain Greece France Italy Portugal And Dubai Which News

Antigen And Molecular Tests Types Of Covid 19 Tests

Rapid Covid 19 Testing Urgent Care Omaha Bellevue Ne Clinics

Covid 19 Testing Gohealth Urgent Care
Racgp What Role Should Antigen Tests Play In Australia S Covid Response

Five Things To Know About The Cost Of Covid 19 Testing And Treatment Kff

Home Tests Could Help In The Fight Against The Coronavirus So Where Are They The Washington Post
Antigen Testing For Covid 19 Is Now Available In South Africa Discovery

Rapid Covid Tests What You Should Know About Accuracy

Covid 19 Testing For Kids Children S Healthcare Of Atlanta
How Much Does A Rapid Covid 19 Test Cost Without Insurance Mira
Posting Komentar untuk "Does Health Insurance Cover The Rapid Covid Test"