Does Neighborhood Health Plan Cover Covid Testing
No matter which MassHealth coverage type or health plan you have MassHealth will cover testing and treatment for COVID-19 at no cost when medically necessary and ordered by your health care provider. To get tested you can go to any COVID-19.
Neighborhood Health Plan Of Rhode Island Home Facebook
Most health insurance plans do not cover COVID-19 tests for reasons other than diagnosis or treatment by a health care professional.

Does neighborhood health plan cover covid testing. These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan. On February 26 2021 the Departments of Health and Human Services Labor and Treasury issued new guidance on the coverage of COVID-19 tests. Department of Labor DOL Department of Health and Human Services HHS and Department of the Treasury have released FAQs to assist group health plans in understanding and complying with the COVID-19 testing requirements under the Families First Coronavirus Response Act FFCRA and the Coronavirus Aid Relief and Economic Security CARES Act.
These tests are only covered when required by applicable law and adjudicated in accordance with the members benefit plan. But Ponce who just graduated has none which means her testing options are more limited. Food and Drug Administration FDA-approved COVID-19 tests and services related to the furnishing or administration of the tests on a first-dollar basis meaning before a participants deductible is met and without requiring any other cost-sharing such as copayments or coinsurance.
Insurers must also provide free antibody testing for COVID-19 patients under the Coronavirus Aid Relief and Economic Security CARES Act. Testing on admission to inpatient or day case procedures are covered. Health insurers must cover diagnostic testing for COVID-19 when ordered by a licensed or authorized health care provider regardless of whether you have symptoms or may have been exposed to the virus.
Health insurance is supposed to cover the cost of your COVID-19 test. You do not need to have symptoms or to have been exposed to COVID-19. The Health Departments mobile laboratory provides testing in locations throughout the county for individuals who are experiencing symptoms of COVID-19 or who may have been exposed to COVID-19.
You are not responsible for any deductible copayment or coinsurance for the COVID-19 diagnostic test. Sites were selected based on Health Department data to increase access to testing in areas within the county with higher numbers of cases and limited testing resources or clinics. Agency guidance has elaborated on these requirements and created new flexibilities to encourage COVID-19 diagnosis and treatment.
COVID-19 relief legislation requires employer-sponsored group health plans to cover certain testing and related items without cost sharing. Members will also not pay a visit fee to a PCP urgent care center or ER if they are tested for COVID-19. At this point I dont know.
The Sa cramento County Department of Health Services is partnering with local community agencies to provide Community-Based Testing Sites for free COVID-19 testing for Sa cramento County residents. Members will not pay for a COVID-19 test. Getty Images By Sara Heath.
Kaiser Permanente is dedicated to meeting the healthcare needs of our members physicians and staff and communities during the COVID-19 epidemic and beyond. Humana Commercial Group members those who receive insurance through their employers will be eligible for COVID-19 testing with no out-of-pocket costs when an FDA approved or emergency use authorized COVID-19 test opens new window including at-home tests has been ordered by a physician or other licensed healthcare professional because the member. Geisinger Health Plan GHP is waiving member cost-sharing for testing and treatment of COVID-19.
To get tested you can pre-register or walk-ups are also taken. You do not need to be an essential worker to get tested. Health Alliance Plan HAP a Michigan-based nonprofit health plan today announced that it will waive cost-sharing associated with laboratory testing for COVID-19 also known as coronavirus.
The FFCRA requires group health plans to cover US. Does my health plan have to cover my COVID-19 test. Federal guidance requires health plans to provide testing at no cost to everyone.
Testing Kaiser Permanente COVID-19. Our Health Care Hacker Jonathon Hess. Food and Drug Administration FDA approved COVID-19 home tests that you buy at a pharmacy or store without a prescription or order from a licensed health care professional are not covered by your plan.
UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. Antigen testing not related to eligible claims andor as part of an individual insurance contract are not covered. Yes if youre experiencing COVID-19 symptoms you think you were exposed to someone.
Promulgated an emergency regulation regarding health plan coverage for COVID-19 diagnostic testing during the state of emergency proclaimed by the Governor on March 4 2020 in response to COVID-19. UnitedHealthcare health plans do not cover COVID-19 surveillance testing which is testing used for public health or social purposes such as employment return to workplace education travel or entertainment. Watch this quick video to learn how to self.
One of the most pressing questions. As a Kaiser Permanente member you wont have to pay for costs related to COVID-19 testing. HAP members who are tested for COVID-19 will not be subject to.
The PCR and Antigen t ests will be administered with a self-administered nasal swab. The health payer will provide at-home or drive-thru COVID-19 testing for members who are displaying symptoms of or at-risk for the disease. Plans and insurers do have to cover at-home testing for COVID-19 under Section 6001 assuming the test meets the criteria in Section 6001 and that the.
Does my health insurance cover testing and treatment for COVID-19. If a member is hospitalized for COVID-19 all in-network inpatient treatment costs will be waived. If youre diagnosed with COVID-19 additional services including hospital admission if applicable will be covered according to your plan details.
Bupa Occupational Health Limited separate from Bupa insurance offers Covid-19 antibody tests to anyone at 65 per person. If you have symptoms of COVID-19 or have been exposed to someone with COVID-19 call your health care provider to discuss getting tested. Per guidance from the Centers for Medicare Medicaid Services CMS the Department of Labor and the Department of the Treasury all Commercial Medicaid and Medicare plans must cover COVID-19 serological antibody testing with no cost-sharing.
Local Covid 19 Testing Options College Of Public Health Uga
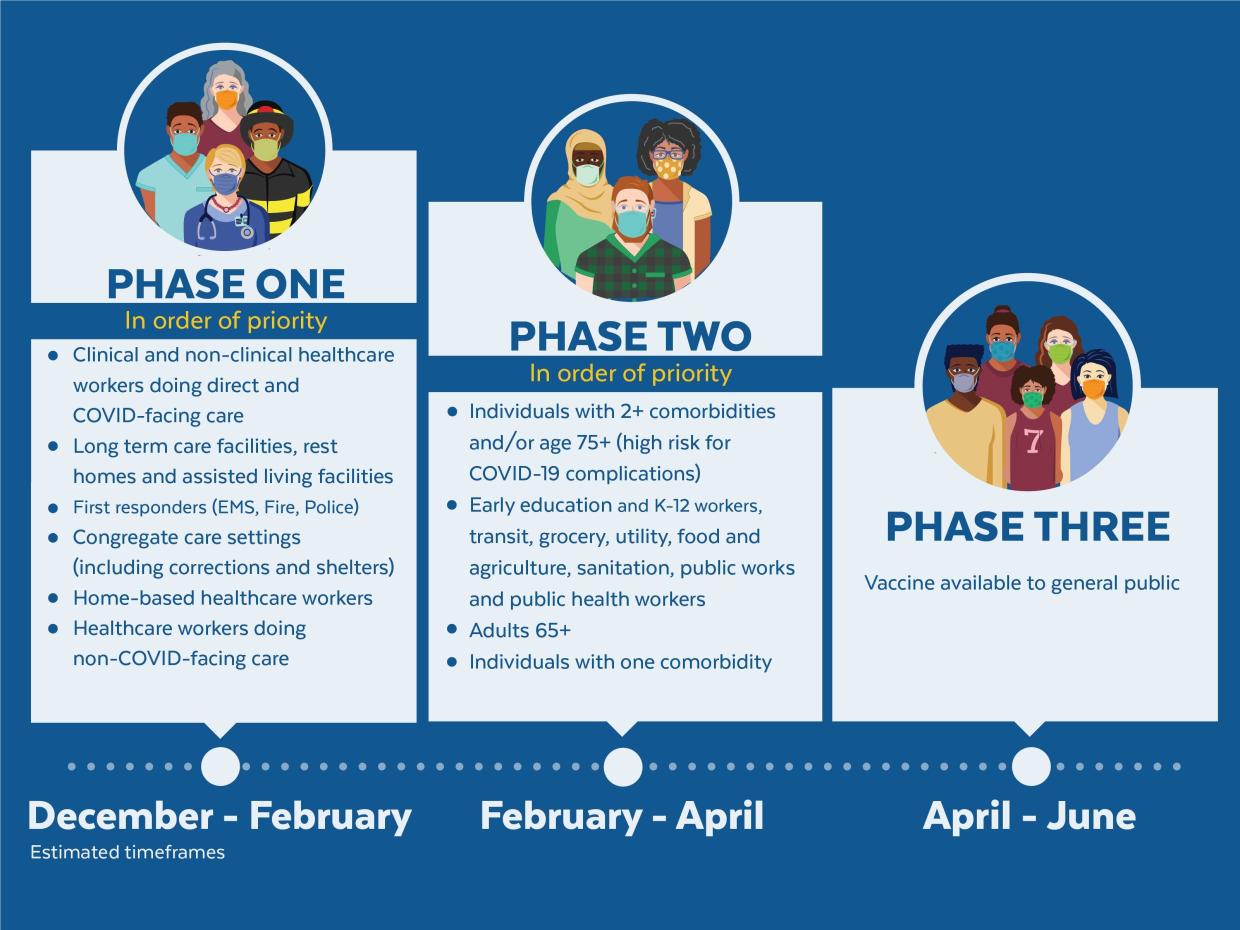
Covid 19 Vaccine Information Community Health Programs
Athens Neighborhood Health Center Home Facebook
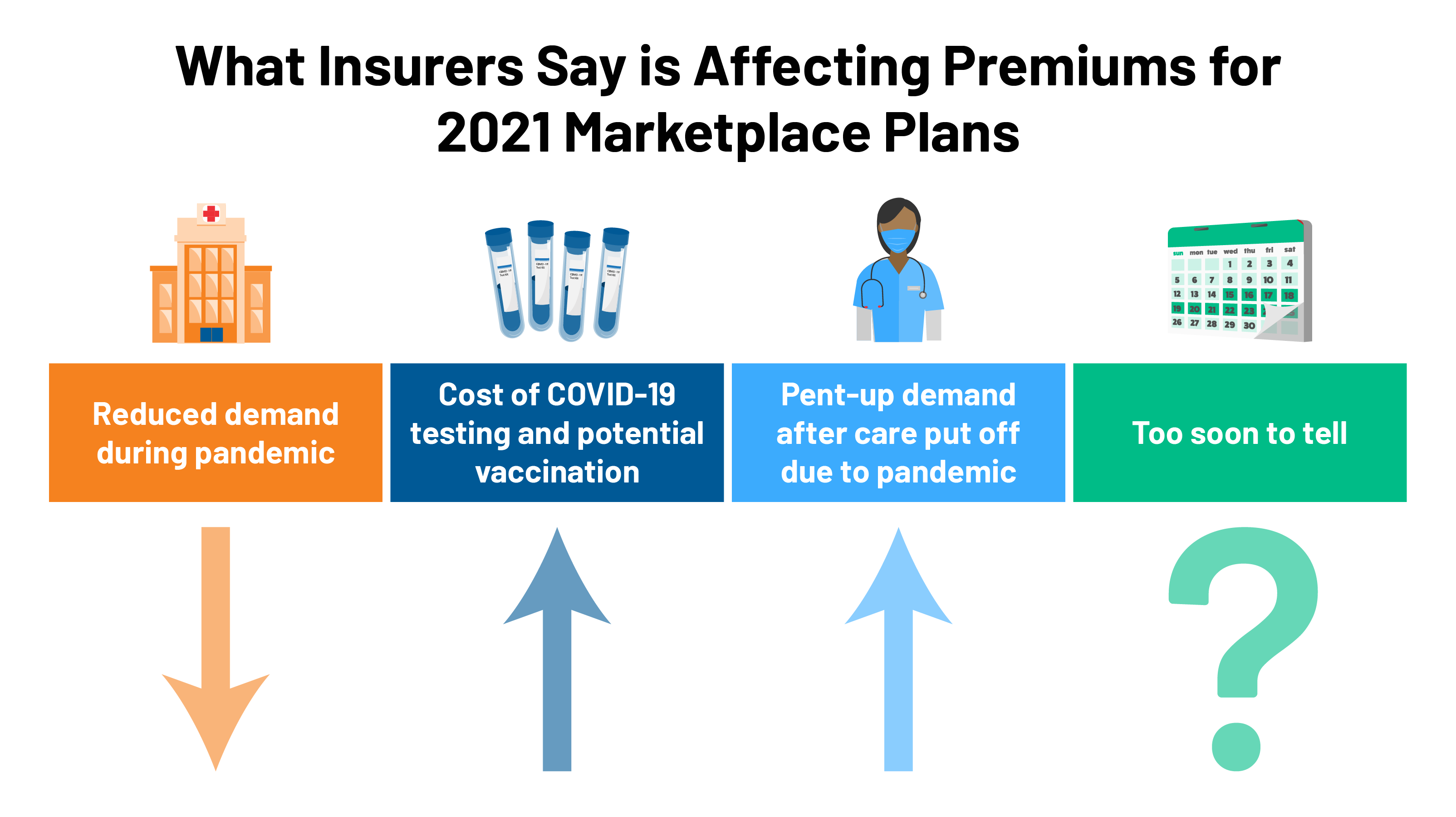
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Home Harvard Street Neighborhood Health Center
Neighborhood Health Plan Of Rhode Island Home Facebook
Pittsfield Neighborhood Health Center Community Health Programs

Covid 19 Get Tested City Of Alexandria Va
Neighborhood Health Plan Of Rhode Island Home Facebook
Neighborhood Health Plan Of Rhode Island Home Facebook
Mattina Neighborhood Health Center Buffalo Ny









Posting Komentar untuk "Does Neighborhood Health Plan Cover Covid Testing"