Will Cigna Cover Covid Testing
Diagnostic testing for COVID-19 molecular or antigen diagnostic tests including rapid tests saliva tests etc is covered without cost-share prior authorization or other medical management requirements through October 17 2021. COVID-19 Vaccine Coverage Regardless of Insurance Status.
A UnitedHealth Group digital tool that enables organizations to gauge predicted outcomes of COVID-19 testing approaches on their populations helped guide a Washington DC schools testing.
Will cigna cover covid testing. Your plan will cover diagnosis testing and treatment associated with COVID-19 including. In general at present tests for COVID-19 are limited to suspected cases and depend on local laboratory testing recommendations. Other reasons for testing such as Employer Mandated Testing may not be covered by your insurance unless under these circumstances.
HR6201 does not apply to short-term health plans healthcare sharing ministry plans or other health plans that arent considered minimum essential coverage. List of Insurance Payers Who Cover 72 hour Results. As federal guidelines continue to evolve in support of the COVID-19 pandemic we proactively extended applicable customer cost-share waivers and other enhanced benefits through February 15 2021 for treatment and through October 17 2021 for testing and testing-related services unless otherwise mandated by the state.
The CARES Act requires health insurance to cover 100 of the cost for COVID testing for those experiencing symptoms or who have concern for exposure. Yes your insurance will cover all costs for the COVID test. Medicaid will cover the full cost of COVID-19 testing for the uninsured as directed by the CARES Act.
The company will not require prior authorization prior certification prior notification or step therapy protocols for these services. We process all COVID testing through your insurance company. Please be aware that separate cancellation cover for Coronavirus is included when you choose travel insurance.
Must administer COVID-19 vaccine regardless of the vaccine recipients ability to pay. This company is a fraud - misleading people during a time like this. The federal government had to step in to require self-insured plans to fully cover COVID-19 testing and to address the issue in the states that hadnt taken action on their own.
BCBS GIC-Unicare Tri-Care Tufts Carelink Cigna Harvard Pilgrim and Medicare. I checked last month on their website to see if they would cover the costs of a covid-19 test. Medical insurance provider will provide coverage of COVID-19 PCR tests when prescribed by a medical practitioner.
Cigna Health does not specify a limit on the number of COVID-19 tests it. On July 19 2021 the Secretary of Health and Human Services HHS renewed the national public health emergency PHE period for COVID-19 through October 17 2021. Physical exams are a wellness visit with no cost to you.
We are a participating provider with several insurance companies. Cigna and Humana have waived co-payments co-insurance and deductibles for all COVID. USAA will cover COVID-19 related testing expenses not covered by Medicare for services received on or after Feb.
And I got billed 150 because Cigna said they dont cover Covid-19 testing. Centene will cover COVID-19 testing and screening services for Medicaid Medicare and Marketplace members and is waiving all associated member cost share amounts for COVID-19 testing and screening. Out-of-Network and Cash Pay sports and school physicals.
Will my insurance cover the cost of a test for COVID-19. Your global medical plan will most likely cover the cost of coronavirus testing if you get a doctor to certify your symptoms and refer you to testing. GeoBlue as an example provides coverage with no cost-share for diagnostic testing for the virus known officially as COVID.
If you require the test for a surgical clearance OR are symptomatic or have had suspected or direct exposure Cigna will still cover 100 of the cost of the testing. Quest Diagnostic COVID test RT-PCR This lab-based test is the gold standard for determining an active SARS-CoV-2 infection and will meet travel requirements. USAA will comply with all applicable federal and state regulations regarding coverage for COVID-19 related services.
The following insurances will cover for Rapid Antigen testing if a patient meets testing criteria. AMERIHEALTH EPO AMERIHEALTH HMO AMERIHEALTH PPO BEECH PPO CHN CIGNA HMO CIGNA PPO CLOVER MEDICARE GEHA GREAT WEST HORIZON ADV EPO HORIZON DIRECT ACCESS HORIZON HMO. They claimed they did.
Be sure to check with your insurance company to find out whether or not they will cover services provided at UHS. Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers whether at a providers office urgent care center emergency room or via virtual care through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. PCR Antigen Antibody Biofire repiratory panel and more Our coronavirus PCR processing equipment will deliver your results within 3 hours.
Our Travel Insurance policy will only provide cover for any claims caused by or relating to Coronavirus Disease COVID-19 or any mutation of under the Emergency medical associated expenses section of your policy book. Cigna Foundation Expands Commitment to Help Thousands of Students Educators and Families Access Healthy Food Mental Health Support Supports back-to-school efforts with programs at 16 schools focused on eliminating food insecurity supporting social and emotional wellbeing teaching resiliency or reducing student loneliness. All organizations and providers participating in the CDC COVID-19 Vaccination Program which currently includes any provider administering COVID-19 vaccine.
Cigna recently changed its coverage for COVID-19 testing. How is Cigna covering COVID-19 testing. Then I got a covid-19 test and provided my Cigna insurance.
According to its website Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing through Jan. CI will repurchase 20 billion of common stock through accelerated stock repurchase agreements the ASR Agreements with each of. Consistent with the new end of the PHE period Cigna is extending cost-share waivers for COVID-19 diagnostic testing and related office visits through October 17 2021.
FG Rapid is the Covid-19 testing site of choice for many South Florida Businesses and travelers. Cigna was the first in its industry to waive customer cost-sharing for COVID-19 testing and continues to protect customers from surprise out-of-network bills increase the accessibility and. Global health services company Cigna Corporation NYSE.
In-network FREE school and sports physicals for your youth are for Aetna Blue Cross Blue Shield Cigna Scott White Health Plan United Health Care and Humana plans. Please see FAQ from Cigna. Please call our insurance specialist at 410-455-3221 to determine whether or not UHS participates with your plan.
We do our best to respond to phone messages within.

Building An Innovation Culture With Cigna Health Insurance Board Of Innovation

Cigna Makes It Easier For Hospitals To Focus On Covid 19 By Helping Accelerate Patient Transfers Mar 23 2020 Cigna Newsroom

The Cigna Covid 19 Global Impact Study Looking After Well Being In Lockdown Health Blog Cigna Europe

Cigna Raises Financial Forecast For 2021 Despite The Ongoing Covid 19 Pandemic Healthcare Finance News

Cigna And Humana Waive Coronavirus Treatment Costs

Cigna Protects Its Workforce By Requiring Covid 19 Vaccinations Or Testing For Employees Entering U S Worksites

Cigna Sees Larger Impact From Pandemic To 2021 Earnings Reuters

Guidelines For Working During Covid 19 Cigna
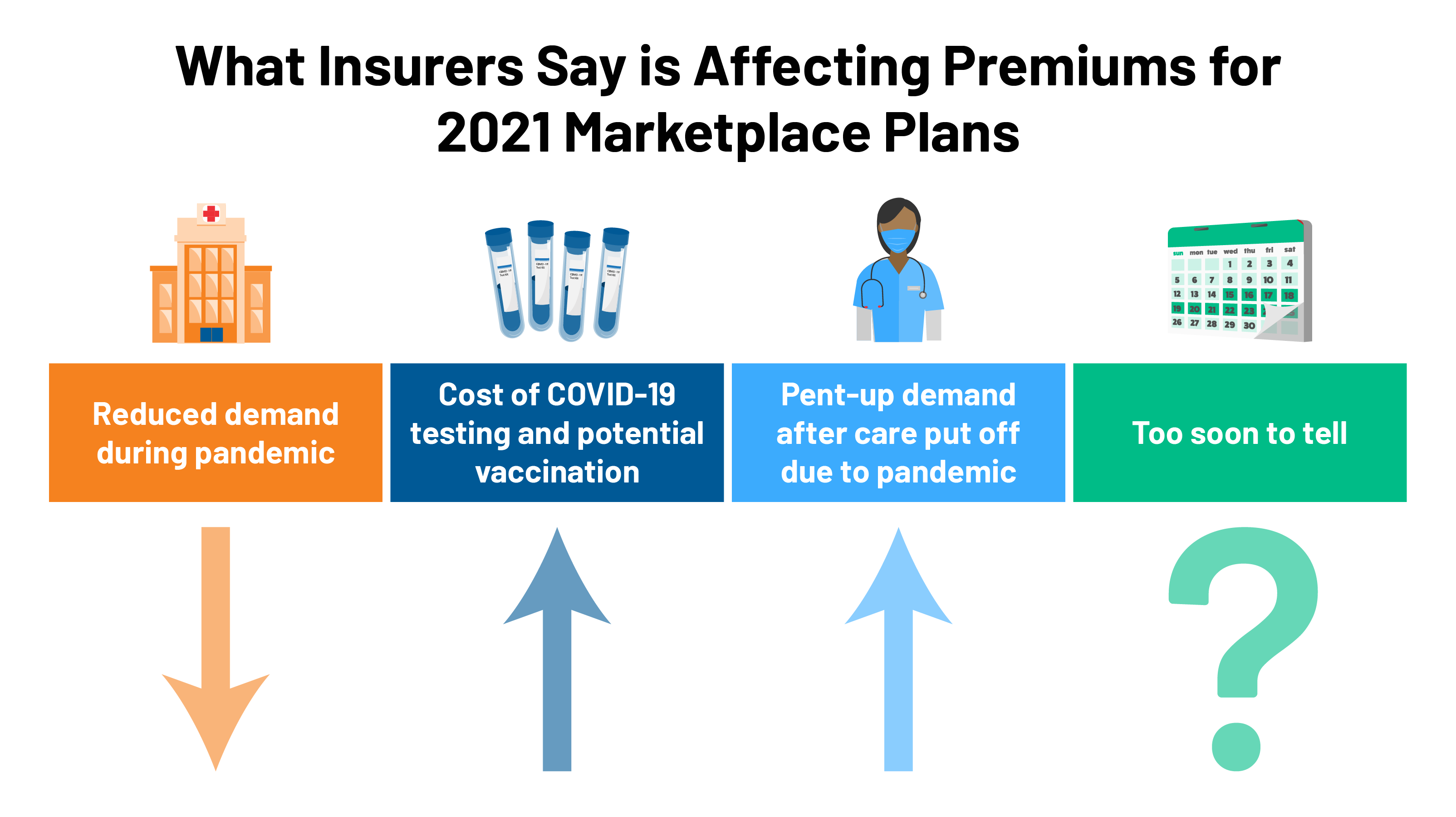
2021 Premium Changes On Aca Exchanges And The Impact Of Covid 19 On Rates Kff

Most People Won T Have To Pay For Covid 19 Testing Coronavirus
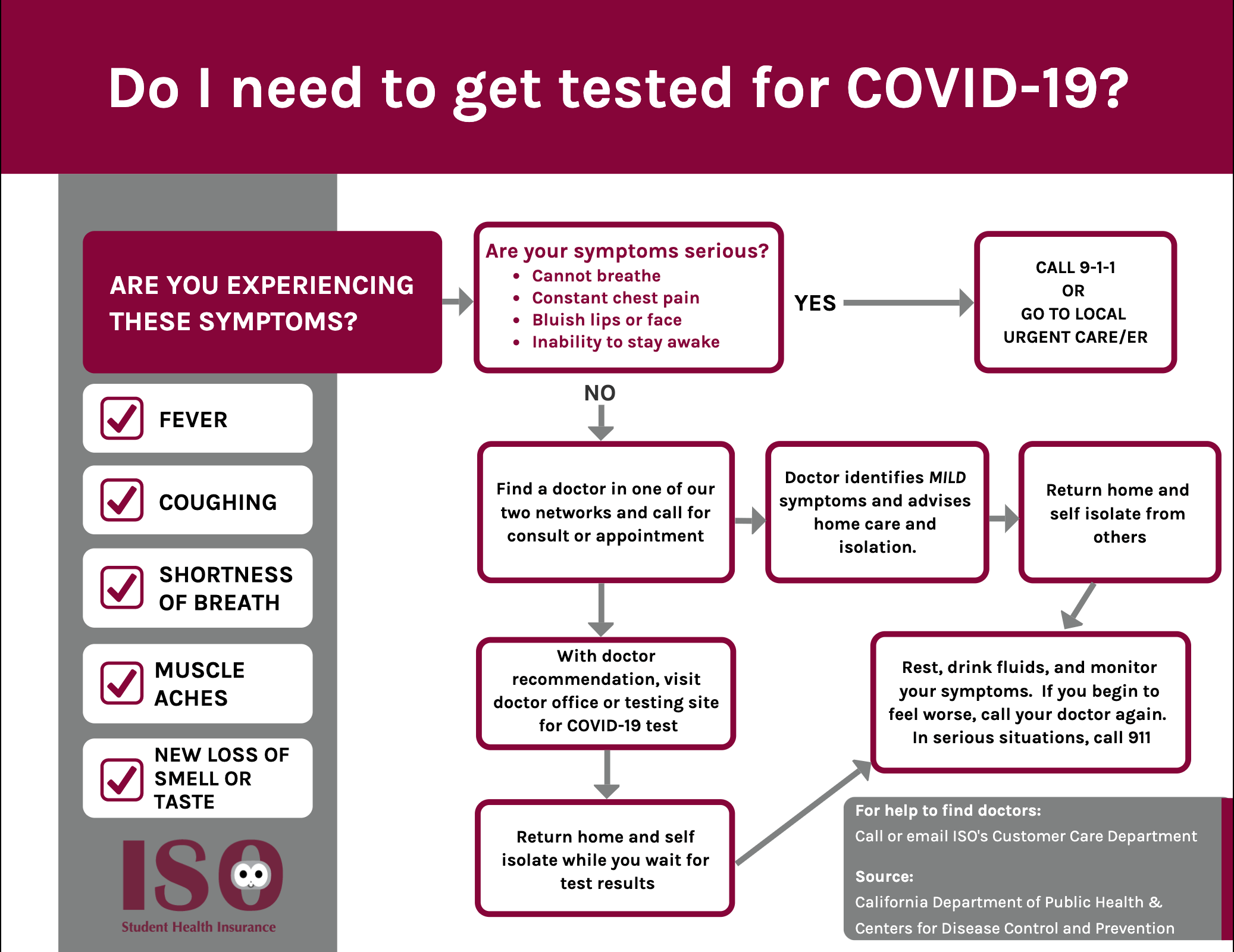
Iso International Student Insurance
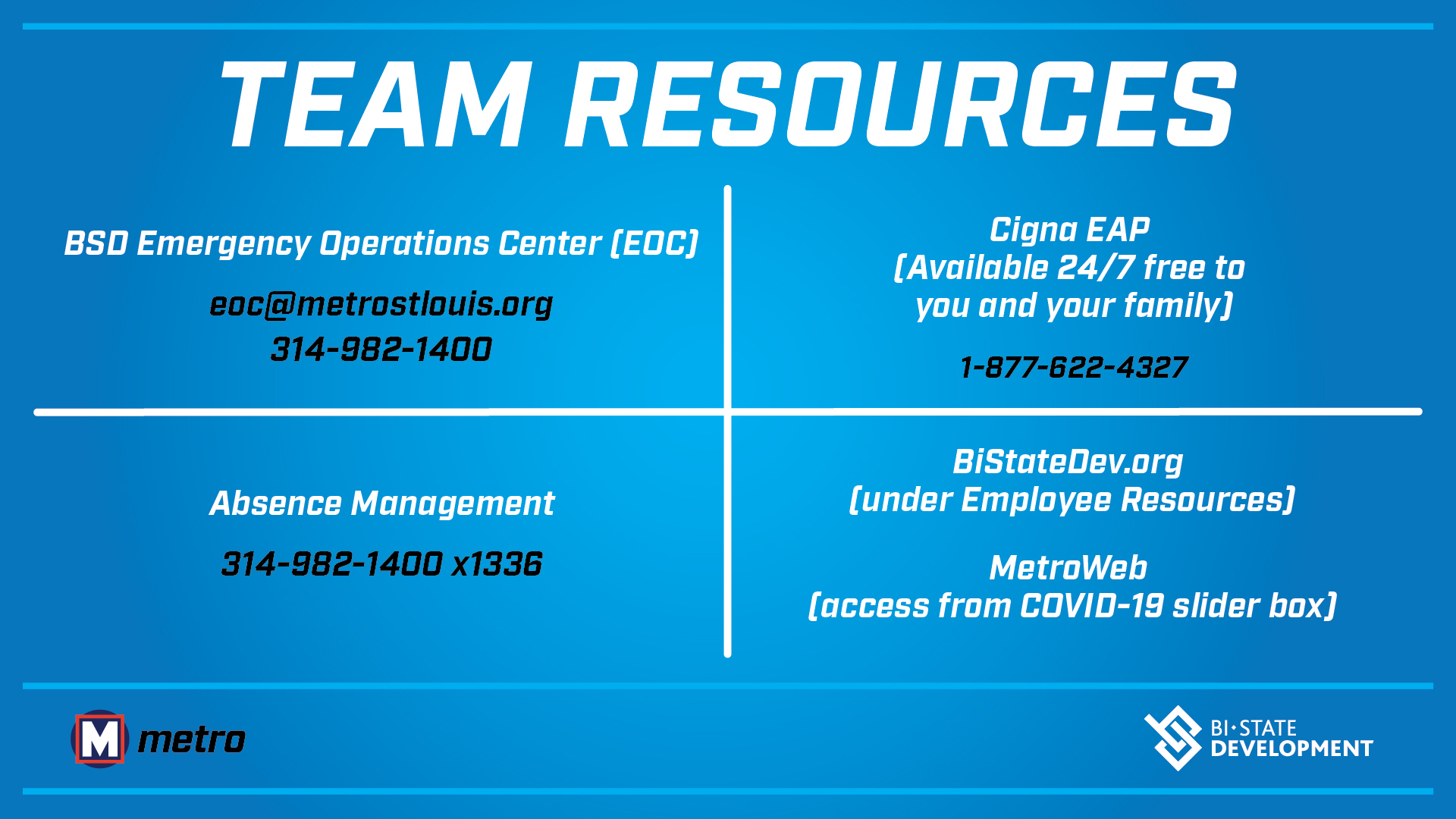
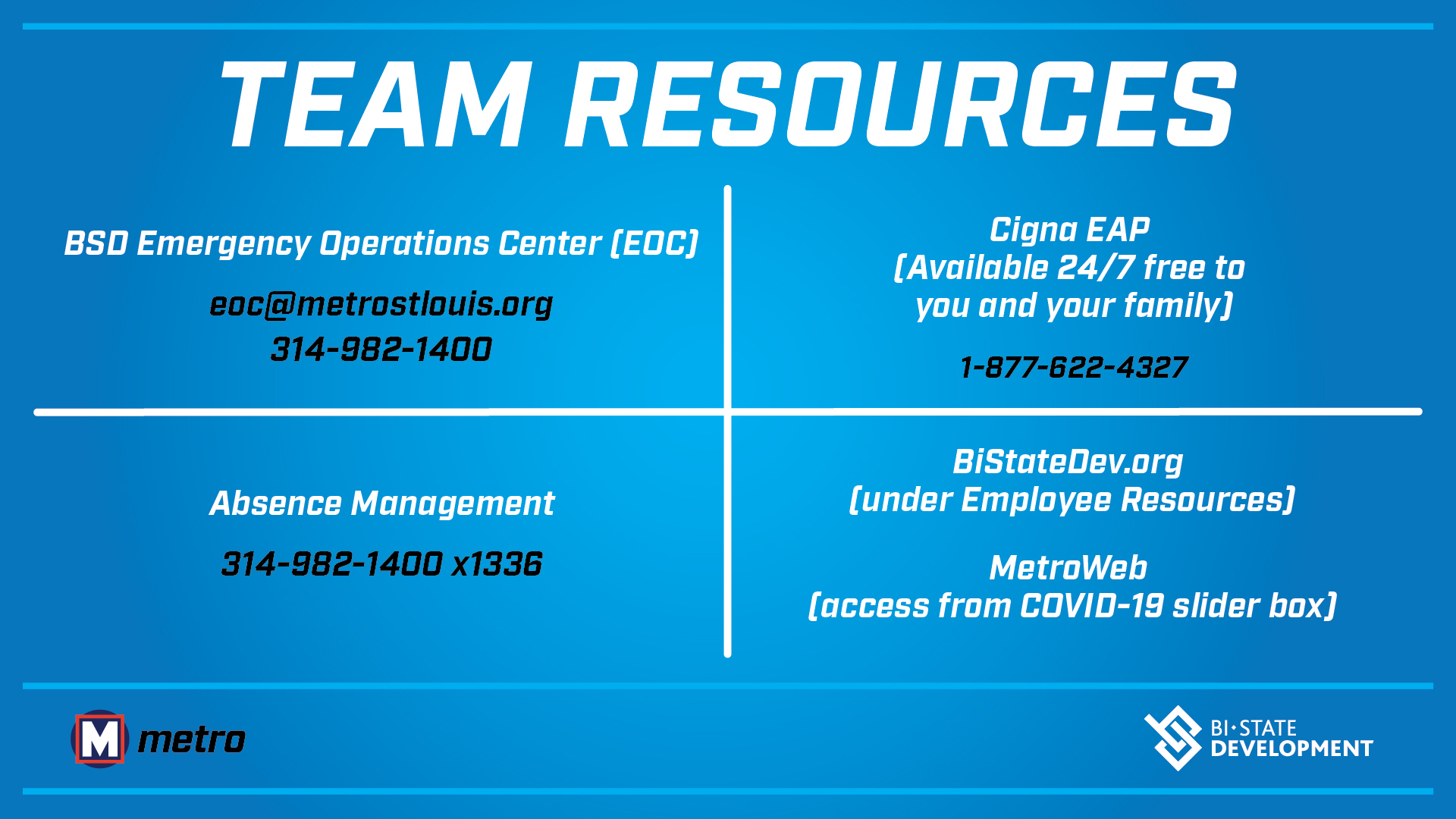
Coronavirus Covid 19 Information Bsd
Posting Komentar untuk "Will Cigna Cover Covid Testing"