Does My Cigna Health Insurance Cover Covid Testing
Private insurers generally must waive an insurance plan members cost-sharing payments for COVID-19 diagnostic testing and certain related items and services as well as COVID-19 vaccine administration. In all cases providers should bill the COVID-19 test with the diagnosis code that is appropriate for the reason for the test.
Or public health surveillance and antibody tests are not covered by Cignas standard coverage but may be covered as required by state law.

Does my cigna health insurance cover covid testing. Cigna covers out-of-pocket expenses for a covered COVID-19 diagnostic visit and testing with no customer cost share through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. Oscar does not cover COVID-19 antibody tests if they are administered outside of these settings because they are not used to diagnose COVID-19 or determine a course of treatment. This is because insurance companies will consider COVID-19 as a pre-existing condition.
We only cover the cost of PCR testing when requested by a medical professional. CI customers will have access to coronavirus COVID-19 testing as prescribed. Connect with a provider.
Under the Families First Coronavirus Response Act Medicare Medicaid and private health insurance plans are required to fully cover the cost of COVID-19 testing. You may also have to fill out a screening form. You have options Cigna is waiving out-of-pocket costs for COVID-19 visits whether.
Please note that routine and non-emergent transfers to SNF. COVID-19 testing at temporary or pop-up testing sites is covered by Blue Shield and Blue Shield Promise without out-of-pocket costs. Access testing if you need it Cigna is waiving out-of-pocket costs for FDA-approved COVID-19 diagnostic PCR and antigen testing tests.
BLOOMFIELD Conn March 5 2020 PRNewswire -- Cigna NYSE. They do not have a lot of openings for unscheduled visits walk or drive-in. But plans that arent considered minimum essential coverage arent required to cover COVID-19 testing.
This exclusion includes cancellation claims as a result of the UK Foreign and Commonwealth Office FCO advice where there is advice not to travel to an area or a particular country. Yes most likely you can still get health insurance if you have been diagnosed with COVID-19 but the insurance company might exclude Coronavirus from your coverage. Per usual policy Cigna does not require three days of inpatient care prior to transfer to an SNF.
Some private insurers including Humana Cigna UnitedHealth Group and the Blue Cross Blue Shield system have agreed. Shots - Health News Congress required health plans to fully cover COVID-19 testing but insurance companies are starting to argue they should only have to pay if patients show. It Depends.
Cigna is waiving out-of-pocket costs for COVID-19 visits with in-network providers whether at a providers office urgent care center emergency room or via virtual care through the Public Health Emergency PHE period currently scheduled to end on October 18 2021. Cigna also offers a free web-based interactive symptom checker to assess COVID-19 risk. Plans and issuers are not required to provide coverage for this type of COVID-19 testing.
According to its website Cigna is waiving out-of-pocket costs for COVID-19 FDA-approved testing through Jan. Many insurers youve seen in the news like Blue Cross Blue Shield Aetna and Cigna have announced that if you or someone in your family gets COVID-19 you wont have to pay anything out of. Section 6001 of the Families First Act as amended by the CARES Act requires private health insurance plans to cover testing needed to detect.
Results are available in 1-3 days after sample is received at lab. We do not cover the cost of antibody testing. Domestic customers can quickly receive information regarding the severity of their symptoms and recommendations on next steps for care.
The company will reimburse health care providers at Cignas in-network rates or Medicare rates as applicable. You will be responsible for any testing costs related to non-diagnostic COVID-19 tests and the cost of the visit associated with the test will be covered according to your plans normal cost-share. Cigna will determine coverage for each test based on the specific codes that the.
Through this early-intervention tool US. The treatments that Cigna will cover for COVID-19 are those covered under Medicare or other applicable state regulations. Cigna is waiving out-of-pocket costs for office visits related to testing and diagnostic tests for COVID-19 as required by the CARES Act.
Does Cigna Cover Covid testing at urgent care. You will need an appointment for most of these sites. In Vitro Diagnostic Testing coverage policy for additional coverage criteria.
Cigna is facing a lawsuit arguing it failed to pay a New Jersey medical office for COVID-19 diagnostic testing and treatment according to a complaint filed this week in federal court. Your travel insurance will not cover any cancellation or disruption claims in relation to the coronavirus the illness COVID-19 for overseas trips booked after 9am UK time on 19th March 2020. Through the duration of the COVID-19 public health emergency period.
The Families First Coronavirus Response Act FFCRA was passed by Congress on March 18 and mandated that Medicare Medicaid and private. Cigna covers medical care for COVID-19 treatment subject to standard cost share copay and deductibles. For further details on testing and our policy please refer to Will you pay for the cost of COVID 19 testing below.
Please review our COVID-19. Insurers must cover the cost of the diagnostic testing even if the person just wants for example to be sure that they dont have COVID before visiting friends or family members insurers are not required to cover the cost of widespread COVID testing thats done for public health surveillance or employment purposes although they can choose to collaborate with public health departments or. Cigna Health does not specify a limit on the number of COVID-19 tests it.

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Covid 19 Pruebas Tratamiento Y Cobertura De La Vacuna Cigna

Cigna Protects Its Workforce By Requiring Covid 19 Vaccinations Or Testing For Employees Entering U S Worksites

Does Your Health Insurance Cover You For Covid 19 Cbs News

Most People Won T Have To Pay For Covid 19 Testing Coronavirus

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Cigna Requires Employees Returning To Office To Be Fully Vaccinated Reuters
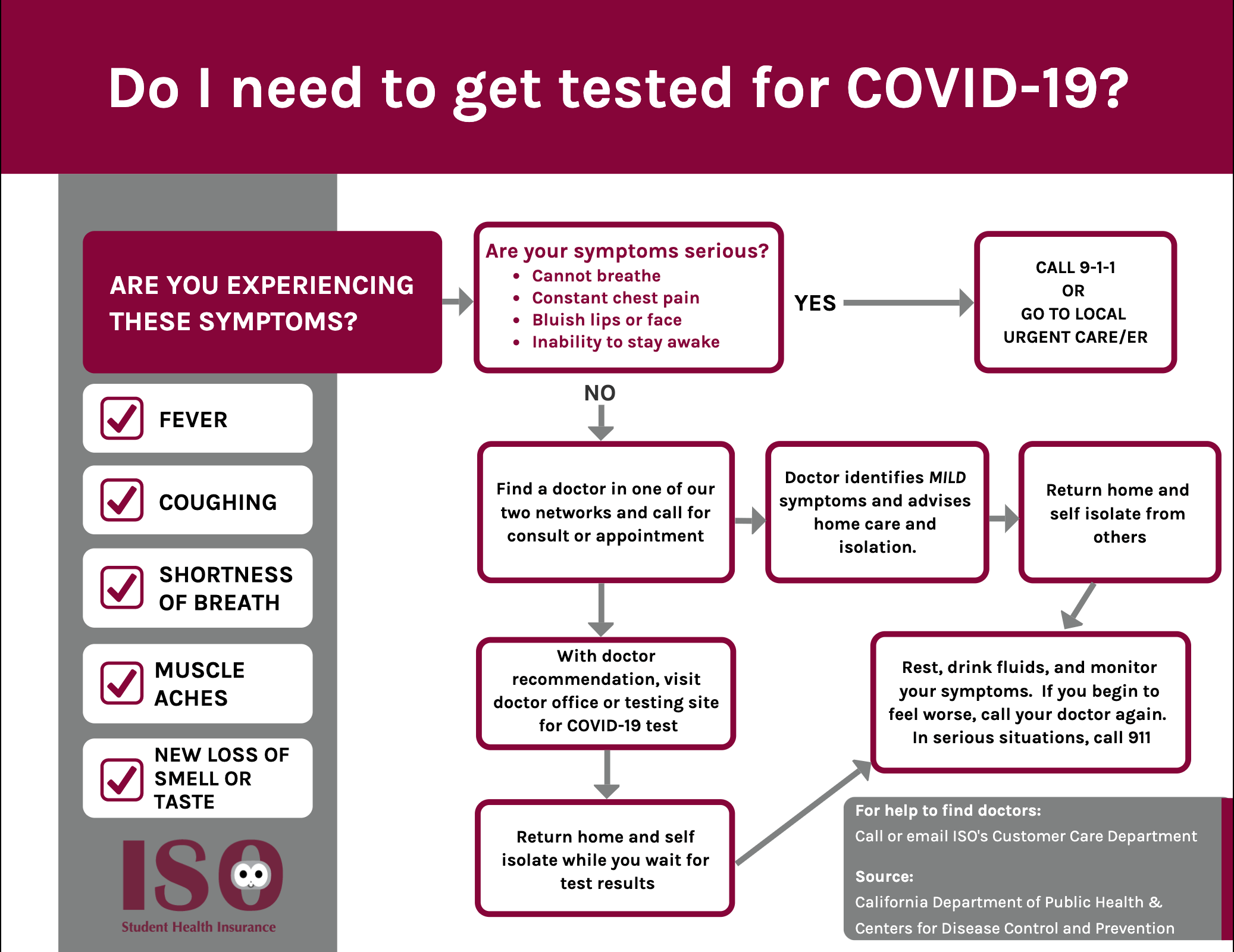
Iso International Student Insurance
Insurance Carecube We Take Most Of Major Insurances

Telehealth Will Be Free No Copays They Said But Angry Patients Are Getting Billed Kaiser Health News

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Centro De Recursos Sobre El Coronavirus Covid 19 Cigna

Cigna And Humana Waive Coronavirus Treatment Costs

Manipal Cigna Health Insurance Plans Reviews And Premium Calculator
Posting Komentar untuk "Does My Cigna Health Insurance Cover Covid Testing"